We’ve Moved!
We’ve moved!
My Psychiatrist Calls Me Back on Sunday! and Introducing BuSpar
Quick update: I’m back up to 1.5 mg of Klonopin as of today. I talked to my psychiatrist, who has always encouraged me to call or email whenever I have a question. He called me back on a Sunday! Yes, that’s right, I have one responsible doctor. Probably because it was Sunday, the conversation was short and sweet: what I am experiencing is too intense. The vivid dreams and night sweats shouldn’t be happening. The high-level daytime anxiety pretty much confirms that it’s Klonopin’s fault. He asked questions like “Have you accidentally forgotten a dose of Effexor? Accidentally doubled up?” But no. I’m super careful. I also have a really dorky pill container with the days of the week, to take even more thinking out of the daily medication routine. I don’t wake up very quickly and sometimes wonder if a conversation or event that took place while I was half asleep did actually happen. I sometimes have to check to make sure I took the meds and counting how many are left in the bottle gets old real fast.

This is what my meds look like in the morning. See the empty "S"? That's for Sunday--yep, I took my meds today.
So here’s the next step: I go on a replacement medication called BuSpar/buspirone. When it kicks in, we try tapering the benzos again, hoping that the anti-anxiety BuSpar will prevent the kind of anxiety I’m feeling with even the smallest decrease Klonopin. This one is “mild,” in the words of my doc, so we’re hoping I can stay on it, even during pregnancy. Let’s switch it out! Adding another chemical is preferable to going through anything like this past week ever again. Because guess what? Pregnant ladies/fetuses and mommies/babies cannot afford to be getting any more bad sleep than they already get and feeling super high anxiety is really bad for everyone. Oh, and that link up there? That’s the Wiki article on BuSpar which, strangely, is the closest thing I could find to what my doc said on the phone. So start there if you’re curious about the drug. Well… Here we go again…
Related articles
- Rethinking Medication and Pregnancy (conceptionquestions.wordpress.com)
- Too Soon to Cry Mercy? I Want My Medication Back! (conceptionquestions.wordpress.com)
- Apprehensive, Excited and Back in Therapy: Good-bye August (conceptionquestions.wordpress.com)
Too Soon to Cry Mercy? I Want My Medication Back!
“I have no talent for certainty.” Jane Austen
It’s been eight days since I tapered my morning dose of Klonopin from 1.5 mg to 1 mg, and it’s been eight days since I had a good night’s sleep. I wake up soaked from night sweats with a jaw clenched so tightly it aches all day. Sometimes I sleep for twelve hours, sometimes for four. I dream about looking for some lost thing or person, but I never know exactly what I am looking for. My nights are full of problems with solutions that seem just out of reach. I just want to go back to eight hours. I want to fall asleep at 10:00 pm and wake up at 8:00 am again. I want to stop grinding my teeth so hard I’m afraid to knock out a filling.
For the first few days, I thought I just had to tough it out. But when I don’t get enough sleep, I get migraines. Understand this: I do not remember ever getting regular, consistent sleep until my early twenties. I remember watching the clock tick past ten, eleven, even midnight, as a child in grade school. (This is a classic sign of childhood anxiety, by the way.) Regular sleep was the first change that helped my anxiety, outside medication. I want my sleep back!
I’m not sure what to do, except ask my psychiatrist if this will end soon. Maybe I need a sleep aid to get me through this time. Maybe we need to make some other change to my medication. But I’m discouraged. I just didn’t see this coming. I expected harder days; I didn’t expect to feel lucky that I only had one migraine in over a week of terrible sleep. I didn’t expect to fall asleep with the kids I babysit in the middle of the day. [For the record, I wake up at the tiniest noise if I’m babysitting. R (18 months) threw one little teddy bear out of his crib, and the sound woke me up.] I didn’t expect to be baking scones at 3 am and watching Dr. Who. Everyone knows that’s a daytime activity!
In the meantime, I think today I’ll go for a very long bike ride and hope that wearing myself out physically helps. Any other suggestions?
Previous related posts:
- Rethinking Medication and Pregnancy (conceptionquestions.wordpress.com)
- Anxiety, Panic & Depression (conceptionquestions.wordpress.com)
- Apprehensive, Excited and Back in Therapy: Good-bye August (conceptionquestions.wordpress.com)
Save Girlhood! and How I Learned to Accept TV
Two events coincided at an interesting moment yesterday. One: my husband’s dream came true, and Direct TV hooked up the satellite dish that brings him a ridiculous amount of NFL and college football. We haven’t had anything except the XBox hooked up to our TV as long as we’ve lived together, so he’s pretty darn excited. I, honestly, am more excited than I expected. What I didn’t realize was that we were signed up for a two-year contract. Whatever. I now have access to BBC America, and this Anglophile is one happy camper.
So last night, while my husband watched football, I participated in a discussion called Save Girlhood on Twitter. (This blogger is officially media savvy. Well, I’m getting there!) What do we want to save girlhood from, you ask? Why, sexualization, of course. The kind we see in, well, the ads that air during NFL games. But for those of you who are new to this debate, I’ll let this fantastic lady fill you in:
@nancy_newmoon sexuality is the inner person, as the subject and proactive. sexualization is others projecting on you as passive object.
(Nancy Gruver is an “Expert on girls, author: How to Say It To Girls, Founder: Daughters.com & ad-free @NewMoonGirls Safe Social Network & Magazine for age 8+ http://www.newmoon.com http://blogs.newmoon.com/parent-girls” – from her Twitter profile. I have loved New Moon since I was small.)
Read this blog, in its entirety, or, if you don’t have time, this post on Lingerie for Little Girls (not a joke) will fill you in on what exactly we’re up against. What does TV have to do with it? Well, I want to have a kid, right? And this isn’t just about girls. It’s also about the messages we send boys about girls. So whether I have a boy, a girl or both, this matters. Here are some highlights from last night’s conversation about the media and its role in the sexualization of girls:
@DrRobyn: Q3: I’m a fan of actually taking the media, toys, etc and showing #girls the problems. discussing them.
@DrBeckerSchutte: when we teach our girls to be critical of media, we give them tools to push back against peer pressure.
@MauveDinosaur If their peers and media is all they have, that’s all they see.
@KnowldgeLinking: Want another shocker? 29% of kids age 2-3 have TV in their bedrooms. 43% of kids age 4-6 do
@DCalifornia: I think TV is a wonderful conversation starter. Good or bad, talk about it, discuss it, point out why it is or isn’t ok
@TheMomarchy Watching TV w kids is one of the best strategies. Called “co-viewing” in research.
I have never been sure what I think about kids and TV. Obviously, TV is not a babysitter. Unsupervised TV is not an option. A DVR will allow us to remove the commercials. [FYI: Kids can’t tell the difference between the program and the commercials! They don’t have that necessary “this is an ad, and advertisers lie to me” automatic response!] For most of my childhood, we watched movies but didn’t have channels via cable or satellite. I think that this was probably for financial reasons. I’m thinking maybe having TV in our house isn’t such a bad idea, with limits and not in the bedroom and, for many years, watching with the kids. I reserve the right to change my mind at any time. Well, I reserve the right to ask that we do not renew the contract. But even if we decide not to pay for this after we have a kid (and let’s face it–there are lots of things we won’t be able to pay for after we have a kid), our children will encounter the crap that’s on TV, and the good stuff too, somewhere. It’s just so accessible. And that’s now–I am going to have to know a lot about what is out there if I want to have a conversation with my child when she or he is ten years old. In 11+ years, it’s just going to be easier to get access to anything we try to ban.
“BPA is illegal now, isn’t it?” NOPE.
From Healthy Child, Healthy World and AP:
“Better labeling news comes to us from Washington state, where a new law went into effect this week that forces manufacturers of toys, cosmetics, jewelry and baby products to report to the state if their products contain hazardous chemicals such as formaldehyde, bisphenol A and phthalates, according to the Associated Press.
P.S. On the BPA front, California is well on its way to passing a law banning the substance from baby bottles, sippy cups, infant formula and baby food.”
Know what that means?
- California has NOT YET banned bisphenol A from baby bottles, sippy cups, infant formula and baby food. (Please tell me that means formula and baby food containers!)
- In Washington state, you can use “formaldehyde, bisphenol A and phthalates” in baby products. You just have to LABEL it, now.
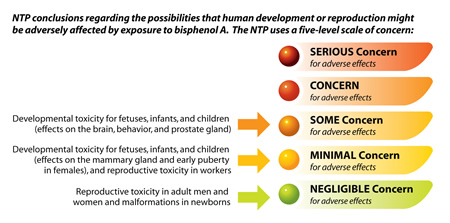
Concerns about BPA are on the left. The level of concern is in handy stoplight color. This is the most conservative statement about concerns surrounding BPA, from the National Toxicology Program.
In case that’s hard to read, there is “some concern” (that’s orange, or yellow-turning-to-red: consider stopping!) for “Developmental toxicity for fetuses, infants, and children (effects on the brain, behavior, and prostate gland).” How? Well, it’s an “endocrine disruptor.” Which means that it messes with hormones (endocrine system). And here’s another tip from the NTP–if you’re concerned, avoid plastics with the recycle codes 3 and 7. The ones that look like this:
These charming folks would like to assure you that your BPA intake is very low, and that there is therefore, no need to worry. Not true. As Annie Murphy Paul writes, in her book Origins, in this case, traditional views are not helpful, because with endocrine disruptors, “the dose does not make the poison.” In fact, a tiny amount might be more dangerous than a large amount. According to Paul, a tiny amount of an endocrine disruptor fails to trip immune system “alarms”–it looks a lot like a natural hormone. If you drank it, undiluted, I’m not sure what would happen, but your body would definitely say “That’s a foreign substance!” and fight it. But we’ve known for awhile now that endocrine disruptors are more dangerous in smaller amounts because they sneak past those alarms and make it straight into breast tissue, umbilical cord tissue, and other scary places.
And just in case you thought you were safe because you use a stainless-steel water bottle and avoid plastic dishes, there’s one more dirty little BPA secret: it’s in your soup can. I have signed two petitions trying to get Campbell’s to stop putting it in their cans; they refused to respond to either. And guess what’s got the highest concentration? Chicken soup. That’s right, the stuff with the character-themed noodles marketed directly to children. Also, ravioli and BABY FORMULA. Okay, enough yelling. But seriously, if you don’t believe me, read this from the Environmental Working Group.
So if you’re one of the people who told me, after my earlier post, that it’s okay to relax, BPA has been banned, this one’s for you. It has not even been banned from baby bottles in all states. True, far fewer baby bottles have BPA in them, but chicken soup and infant formula cans still have it.
Send a letter to your senator. Ask that our kids be protected from BPA. The smart people at MomsRising.org, “where moms and people go to change our world,” have already written a great letter for you. All you need to do is sign it.
No, I’m Not Pregnant, but Since You Ask…
It could be worse. People could keep asking me if I’m pregnant because I look pregnant. I don’t, and I proved it today, when the cooler weather allowed for the reappearance of my best jeans. People ask me if I’m pregnant because, let’s face it, I’m begging them to ask. I use my Facebook page to promote a blog about conception. I use “pregnancy” in a lot of titles. I belong to online communities composed largely of mothers. I get it. But here, for everyone who hasn’t seen me in a while, is a photo of just how not pregnant I am:
I even added a dreamy filter effect to celebrate the dreaminess that is my pre-pregnancy waistline. (That’s for all of those dreamy baby photos I keep seeing. So there, friends with adorable infants!)
But seriously, I wanted to share this story as a tribute to my marriage:
The baby fever stuff started awhile ago; I don’t remember how long ago. It seems like forever. But at one point, I asked my (then) new Connecticut therapist if she wanted to meet Nathan, to put a face to his name. The three of us ended up talking about my baby daydreams and Nathan’s reluctance to engage with them; he didn’t want to get my hopes up. I knew that it would be awhile before we could practically consider having a child. But he is careful with my feelings, this husband of mine. My therapist had an excellent suggestion, and we agreed to meet back in her office in one year. By then, I thought I could safely taper off my medication and we could be a little more settled, financially. Nathan agreed.
Early next spring, then, we will meet in her office again. We will discuss whether we are ready to start trying for a baby. If we decide that we are not, we will set a date, about three months later, to return and discuss the choice again. The idea, here, is to create a safe space to discuss this delicate issue. We don’t exactly need a mediator, but when I have my heart set on something, a calming influence really can’t hurt. It limits the discussion to an hour. I don’t expect that any surprises will come up; we’ll both know the answer, going in. If the answer is “not yet,” I will need to limit the number of times I allow myself to talk around the circle of reasons why we should wait. If the answer is “yes,” then I’m sure Linda will have plenty of questions for both of us.
I see this as a tribute to the kindness of my spouse, and to his patience with me. If we did not have so much kindness, or if we loved each other less, this year of waiting might be a strain on our relationship. We are able to enjoy each other and our quiet life together. I can honestly say that lazy weekend mornings are sweeter, knowing they might end some time next year. I love that we have all this time to know each other, and our partnership, before making such a big change. No one ever really knows what happens inside a couple’s life together, except the two who share that life, but their children do see an awful lot. I don’t mind holding on to the smaller secrets of our marriage a little longer. They are precious and ordinary, sweet and complex, small and important. I love you, Nathan.
Some related posts:
- Rethinking Medication and Pregnancy (conceptionquestions.wordpress.com)
- Educate Yourself! Read the Pregnancy and Anxiety/Depression Bible (conceptionquestions.wordpress.com)
Educate Yourself! Read the Pregnancy and Anxiety/Depression Bible
Today’s post is a book review with a mission: to promote awareness about anxiety and depression before, during and after pregnancy. I sent a copy of this book to my mother. I will send one to your local library if it doesn’t have a copy. This book is so important. Thankfully, its title is better than “Pregnancy and Anxiety/Depression Bible.” It is my bible, though, and it is actually called:
Pregnant on Prozac: The Essential Guide to Making the Best Decision for You and Your Baby. By Dr. Shoshanna Bennett, Clinical Psychologist.
This is the only comprehensive source about what to do if you already have anxiety, depression, OCD, bipolar disorder, etc. and want to have a baby/are pregnant. I am not exaggerating. Want to read a book about postpartum depression? Everyone and her sister has published a book on it. Take your pick. Lived with this your whole life and want to prepare for pregnancy with that plus an increased risk for postpartum you-name-it disorder? ONE BOOK. One. Many thanks to everyone who has worked to erase the stigma on PPD. Seriously, you have done amazing work. Can we also turn some attention to pre-existing, prenatal & postpartum anxiety? Even the Surgeon General knows that anxiety disorders are more common in women. I can’t help but feel that we don’t have more books about this because people just don’t want to talk about it in general. In my experience, we refuse to talk about something when we are ashamed. In fact, this blog is part of my effort to stamp out my own shame and feelings of failure and inadequacy. Stomp! Stamp! Stomp!
And now, about the book:
Dr. Bennett writes as though her readers were sitting in her office. She has obviously spent a lot of time talking with patients and their families about treatment options and pregnancy. Her extensive experience shows as she relays scientific/medical information in a conversational tone but avoids throwing everything at you at once. Her information is backed by research, but her tone is never cold. Patients’ stories (names changed, of course) sprinkle the text, proving that these decisions are different for everyone. She also calms fears obviously related more to the stigma surrounding mental illness than to reality. This woman is clearly used to talking to real people. The fact that my mother really liked this book says a lot, too, because when she’s worried, she can’t just ask about it at the next therapy session. Relying on me for information can be hard; I used to practice denial like some people practice yoga. This book helped us so much, because it gave us a more neutral place to start talking to each other about the decisions that would come up when I did get pregnant. The more my family knows in advance, the less I have to explain all at once.
You see, there are two distinct parts to any decision I make about my treatment and pregnancy. There’s the medical/psychological part, obviously, where I look at the risks and benefits with my team of professionals, a process I talked about in an earlier post and will talk about again later in this post. Then there’s the part where I explain that decision to close friends and family. My mom, my mother-in-law, my sister, by very closest friends. Don’t get me wrong–not everyone has the right to ask for more information. I don’t mean to imply that women who take antidepressants during pregnancy have to explain themselves. My advice for dealing with self-righteous people who tell you what to do and/or demand that you justify a decision they don’t understand is simple: walk away. My dad likes to say “Don’t argue with an idiot. He’ll drag you down to his level and beat you at his own game.” Most of what my dad says about people in general is unkind and untrue, but I am inclined to agree with his assessment of idiocy. This process I’m talking about, the one that comes after the decision, involves educating the people who love me. They worry. Their hearts are in great places. I want to them to feel included and informed.
There’s a special person in that group: my husband. Dr. Bennett is so eloquent about partners. She has talked to many, because they are necessarily part of her patients’ decisions. Nathan is my everything. I get antsy when he’s away from home. He’ll obviously be the father of any kid I bring into this world. So I gave him a privilege no one else has. I even signed papers to make it legal; he can talk to my therapist and psychiatrist directly. [Time out to say thank GOD these papers exist separately from the marriage contract, so there are no secret phone calls ala Don in Mad Men calling his wife’s psychoanalyst to get a full report on every session. Nathan would never do something like that, but I’m just glad it’s not legal anymore in general.] Nathan has the advantage of being able to come in to the office and ask my therapist or psychiatrist direct questions. He still talks about the time he got to spend alone with Dr. Griffin, my psychiatrist, when they just asked each other questions about how best they can help me. And that conversation is still helpful for me, too, if only because the fact that they know and like one another gives me a great shorthand when talking to them. Nathan’s trust in my “team” has a lot to do with feeling included. But it’s not so easy for all partners. Some of them come into this process for the very first time after one partner is already pregnant and the decision must be made as quickly as possible. Some people don’t even know they have any feelings about medication and pregnancy until they’re staring at an ultrasound. Nathan might experience that. And we have a place to go, an expert to ask, when these heartbreakingly delicate decisions come up. As Dr. Bennett points out, this saves everyone so much heartache. It gives the conversation a safe space and a time limit. No unending circular discussion necessary. I’m not about to invite everyone I’m close to. And I don’t have to, which is great because it sounds exhausting. I can just give them a copy of this book and talk to them after they read it.
A note on building a team: as Dr. Bennett so wisely advises, a team of people who each have expertise in a different area is the best way to go. Therapist and Psychiatrist are, in my case, two members of that team. There’s a whole chapter in Pregnant on Prozac on “The Importance of Therapy” and a subchapter called “Pills Are Not Enough.” I couldn’t agree more. My psychiatrist says he will refuse to write prescriptions if I don’t stay in therapy. He doesn’t think it’s safe to stop checking in with a professional, nor does he believe that true progress is made by only taking pills. There’s no treatment of the underlying problem in that approach. And one unfortunate truth of psychiatry is that pills eventually stop working. [Your body gets used to that chemical, metabolizes more of it, less of it gets to your brain, and you have to find a new one. This is the same reasons why alcoholics need a lot more liquor to get drunk than those of us who almost never drink–the liver takes out more and more of the stuff that makes you drunk before it can get to your brain.] Dr. Bennett feels the same way about therapy: treat the mind, not just the brain chemistry!
But there’s another chapter called “When Professionals Don’t Agree.” This is more and more likely to happen as my team of professionals expands to include experts on each of the things I want help with: therapist, psychiatrist, nutritionist, general practitioner, neurologist. So far, I already have that going. When we visit the Columbia University Women’s Mental Health Center, I’ll add an expert on mental illness, psychopharmacology and pregnancy. When I do actually find myself pregnant, I’ll add either obstetrician, midwife, or both. Then, I’ll add a doula. At the very end, there may be new nurses and doctors in a hospital who become part of the team. I am going to spend a lot of time in a lot of offices! What if they don’t agree? Who should I listen to? I should listen to the person who has the most expertise in that issue.
As Dr. Bennett points out carefully and forcefully, expertise in a field like psychiatry or obstetrics does not guarantee expertise in treating a pregnant woman who has an anxiety or mood disorder. This book confirmed my opinion that my psychiatrist is a great doctor because he says things like “I’m not an expert in pregnancy and antidepressants.” It also had me primed to accept his referral to the experts at Columbia University who are comfortable giving me advice on that topic.
So, what if my nutritionist doesn’t like the idea of me taking antidepressants during pregnancy? She is an expert on many things brain-related, but not on psychiatric disorders. I will kindly ask her to let me make that decision and to focus on my diet. I will look for a midwife or OB/GYN here in New Haven who has experience with pregnant women who have mood disorders, but even if I find such caregiver, s/he might disagree with the Columbia expert about medication during pregnancy. What then? Well, I will give each team member a list of the other professionals’ phone numbers so that they can argue among themselves, if necessary. I will most likely take the advice of the Columbia expert because I will have asked them for advice specifically about medication during pregnancy; I will be asking the midwife or obstetrician to help me with other maternal/child health issues and to be with me during labor/birth. Can you see why this whole Team of Experts idea is a truly great idea? Read the book for more on how to go about building your team, especially for some great advice about how to identify a true expert.
This is a long book review, I know. But as you can see, it’s not just a book review. It’s a compilation of the advice I have so far found most helpful in the pregnancy/medication decision. The first place I encountered most of that advice in one place, in easy-to-read prose, was Pregnant on Prozac. [By the way, she discusses many possible medications, not just Prozac, but it does make for a pithy title, doesn’t it?]
The book is for everyone who is at risk for every kind of mood disorder before, during or after pregnancy. I recommend it to anyone who is at all worried about this issue. Did you know that obsessive-compulsive disorder is relatively common during pregnancy and postpartum? Checking to make sure the baby is still breathing every five minutes is not normal. You should feel nervous but not having panic attacks about taking a new baby outside. I mention this one in particular, because many, many, many people tell women who suffer from OCD during or after a pregnancy that her worries are normal. Yes, it is normal to worry. No, it is not normal to fear nap-time because the baby could just stop breathing at any moment. But it is so hard to see and happens so easily because moods change all the time when hormones go crazy. Wouldn’t it just be great if every woman knew the warning signs of an actual disorder? Wouldn’t it be great if more women could feel free to ask an expert “is this normal?” Wouldn’t it be nice to know that it is normal? And wouldn’t it be really nice to get help if it isn’t?
Psychological screenings are slowly becoming part of routine prenatal and postpartum care. But it’s not happening fast enough. I believe that the best way to make this happen faster is for women to demand that their doctors take better care of their mental health. Go ahead! If you’re pregnant or just had a baby, on your next doctor’s visit, say “I want a psychological screening, just to make sure.”
Here, I’ll walk you through a psychological screening to make it less scary: you sit with a doctor and answer questions about your daily life. Your habits. How you feel about ordinary things. They take notes. Some of the questions sound weird, but they are just questions. Trust me, they want honest answers. They’re not hard questions, but the tricky part is to stop looking for the meaning behind them. That’s a little hard, especially with all the note-taking. But it doesn’t necessarily mean anything. Focus on being as honest as possible, and focus on the question at hand. If they ask “How often do you check on the baby while she’s napping?” then just tell them. If you freak out and ask “What does that mean? Are you saying I do it too often? Are you saying I don’t love my baby?” then they will try to calm you down and bring you back to answering the question. They won’t tell you what it means, so don’t bother asking. Remember that if you give honest answers, you’ll get an honest answer. And that these people deal with liars for a living.But seriously, you know what’s a lot scarier than a diagnosis? Trying to deal with an undiagnosed mental illness all by yourself. Trust me. That’s harder than anything.
Day 3?! Come ON.
It is only Day 3 of the Lower Klonopin Dose. It feels like it’s been a month. It is only half a milligram less than I was taking, but that’s a 30% decrease. Which means that these things happen:
- I get so stressed out about choosing an ice cream flavor and then about the ice cream melting in the car that I ask Nathan why it is fun for him to stress me out and decide that we will not get any ice cream at all.
- I try to ask Nathan for help finding the yogurt-covered raisins and instead stutter something incomprehensible. I have to take a deep breath and a long pause before beginning again and actually succeed in ask the question. I do not have a stutter. Never have. Until today, apparently.
- I am annoyed because I have finished my soda and the grocery store has no recycling in the parking lot. I am so torn up about what to do with the empty can that I forget to take it out of the cart.
- I contemplate calling some sort of health department over the mold in the bathroom ceiling.
- I accuse Nathan of laughing at me at once every hour.
Rethinking Medication and Pregnancy
I want to see what medication-free life is like for a while. –Me.
Psychiatrist: Is that goal separate from having a baby? Do you think you’d still want to “live ‘medication-free'” at this time if you didn’t also want to have

Sorry for the generic photo. But this is what I wake up to every day. This orange bottle that is my savior one day and my albatross the next.
a baby?
WHOA. That is a good question. I did not see that question coming.
It was one of those moments where my brain creaks with effort. Quick! Adjust to an entirely new perspective, right now! Like when you suddenly see the other image in one of those old lady/young lady with a hat optical illusions. It was one of those moments that makes me so proud to have asked for professional help. Because this guy? He knows stuff. Here’s why he asked:
I can’t separate them. I want to get off all medication because pregnant women take vitamins, not prescription drugs. Because there is a warning label on my medication about taking it while pregnant. Because I should. And that information really matters if my doctor is going to do his job properly.
If going off my prescription medication, all of it, were a life goal (a goal separate from anything else), then I could do it with a lot of effort and a lot of time and a lot of patience. I do have a lot of patience. I have the patience to carefully decrease my daily dose of Klonopin, a medication classified as a benzodiazepine–I have been doing this for years. When I met my husband over three years ago, I took two milligrams of this stuff morning, noon and night, for a total of six each day. As of this morning, I take one milligram of Klonopin, once a day. These last few milligrams and half-milligrams are the hardest. The dosage has decreased and increased and decreased again. We’re months from being done. I have patience. But that’s exactly why this is such a great question for the doctor to ask–going off Klonopin was a life goal long before I felt any immediate desire to be pregnant. Which is not true for Effexor, the SNRI I take to help me manage anxiety and depression. Before I wanted a baby, I was just fine with the idea of taking an antidepressant every day for the rest of my life. I have been smart about coming off of Klonopin. I’ve gone slowly and I’ve been patient with myself (mostly) and I’ve been honest with my doctors. Because I don’t feel the same way about the antidepressant–I just want to stop taking it for the sake of a hypothetical fetus–I will not be happy to wait as long as it takes to do so safely. I will be pissed. I will be stomping my feet and hating myself for not being able to do it faster, which will cause more anxiety and slow down the whole process. Not a fun cycle.
And here’s what I knew but did not fully understand until my doctor articulated the idea: it may be safer for the fetus (hypothetical though it is) and for me if I stay take antidepressants during pregnancy. Yes. Taking a prescription drug with a warning label on it might be safer.
How do we figure out if it is safer to take the meds or to not take the meds? A cost-benefit analysis. “Cost-benefit analysis” is an economic term for something we do all the time–weigh the pros and cons and choose the option that costs least. The textbook example (at least in my textbook) was going to college (vs. not going at all). It costs time and money, including the cost of the money you’re not making at a job because you’re in school. You benefit by getting a better job and earning more money in the future. Is anyone else with a fancy college degree and loans to pay wondering about that particular benefit? I liked econ. class. But I also read about applying this concept to life in a great book called Spousonomics: Using Economics to Master Love, Marriage and Dirty Dishes.
It sounds really simple, right? Pros and cons lists are easy! Except that in study after study, we find that human beings are generally bad at being honest about pros and cons. We do things like count “the label is nice” as a “pro” when choosing a brand-name pain-killer over the generic we know has exactly the same ingredients and costs two dollars less. We are famously susceptible to ads featuring beautiful people. We order something at a restaurant because it “looks good” in the picture on the menu even when we know that whatever is in that photograph is probably not even real food. Getting people to do accurate cost-benefit analyses is darn near impossible.
But I can get a lot of help making my list from people who know more about this than I do and have a tiny bit more perspective on the issue. Here’s what I know so far:
- There is evidence that links benzodiazepines to birth defects. There’s a link, but it’s not fate. If I take Klonopin while pregnant, it is more likely that the fetus will have a birth defect. (To the friend who could not stop taking her Klonopin when she found herself pregnant–you are brave and doing so well, even though things get really hard. Your girls are lucky to have a mom like you!)
- The research we have has not found a link between most antidepressants and birth defects.
- Some antidepressants do show an increased risk of birth defects.
- There is a giant body of research that links untreated/unsuccessfully treated depression in pregnant women with harm to the baby. These babies cry more and sleep less than babies born to women without depression or whose depression has been treated successfully. This is true in the first 48 hours and, as a matter of fact, even after many months, the children whose mothers were depressed during pregnancy tend to be more sensitive and less resilient than other kids. Bottom line: out-of-control depression and anxiety during pregnancy is bad for a fetus.
- Both Effexor and Klonopin are habit-forming. (The baby could go through withdrawal after birth if enough of the drugs get through the placenta and into the fetus’s blood stream. I have no idea how likely this is, but I’m throwing it in here because I freaking hate what my body does if I don’t take my meds.)
- SSRIs and SNRIs have been around for a long time, and many women have safely taken them while pregnant.
- No cognitive technique I could possibly use to stop an anxiety attack would counteract the effects of a high “baseline” level of anxiety. This could have already done serious damage by the time I recognized the problem and got help. In other words, going off the SNRI only to go back on it while pregnant is not a pretty scenario. And my “baseline” is high. If you knew me before I was medicated/in therapy, you might remember that I was, well, on edge and a bit moody.
Sometimes, the chemicals our bodies make are worse for a fetus than something artificial. If I can safely stop taking Klonopin, that’s really a good idea. But I do not know if it’s a good idea to try going off of everything, altogether. In this case, “natural” is not necessarily the best.
I might feel overwhelmed by this if I didn’t have an ace up my sleeve. Ready? Drumroll please…
The Columbia University Center for Women’s Mental Health Center
My psychiatrist recommends these people very highly. He says that both Nathan and I can go together for a consultation in which people who specialize in the mental health of pregnant women give us information and advice to help us make decisions. He says that he doesn’t know enough about treating a pregnant woman to comfortably give me the advice I want; so he’s sending me to people who do know.
No matter what I choose, I’m going to be giving up something I have grown really attached to: either I wait to get pregnant or I give up the idea of a prescription drug-free pregnancy. I don’t want to wait. I don’t feel comfortable exposing a fetus to antidepressants. Remember what I said about people being bad a cost-benefit analysis? Here’s another example. A big part of me whispers that if I just threw out the drugs, I’d be fine. Eventually. That part of me is stupid. I feel like utter crap if I skip Effexor for just one day. Toughing it out is not an option.
A therapist once told me that I draw too many “lines in the sand,” meaning that I give myself rules and deadlines that are impossible to follow/meet and then beat myself up for failing. Our current plan is to make a decision about trying for a baby next spring. Which means that I want to start trying for a baby next spring, dammit, and have gotten my hopes up! This is not a line in the sand, though, it’s a safe space. We decided to set a date (March 1, 2012) for making this decision so that we didn’t have to talk about it constantly or wonder what the other person was thinking. But it could easily become a line in the sand if I start thinking that I must come off my medication by March. I have already said things like “I’ll be off Klonopin by December, and then we’ll immediately decrease the dose of Effexor!” I see it now–that’s absurdly difficult. Nathan’s concern about that plan? Valid. Holding myself to a schedule like that could put my health in serious danger.
Another stupid part of me is whispering you are already a bad mother, too impatient to make the healthiest choice. (For the record, this is not an actual voice.) It’s important to articulate that thought. Because you know what? If I decide to wait until my un-medicated baseline level of anxiety is comparable to what I feel now, I might wait forever. So here’s my new world: I might never be comfortable without medication. That is a possibility. I am trying my very hardest to accept that without throwing around the word “Failure.” Like a diabetic who takes insulin during her pregnancy, I might have to take medicine that helps me fight anxiety and depression during my pregnancy. I’d be doing it for me and for the baby.
One picture has been stuck in my mind since last night’s session–it’s a printout from a monitor recording mirror image heart-rates for fetus and mother. It comes from a woman who is suffering from depression and her unborn baby. In a study done at Columbia University, fetal heart rates stayed relatively constant, even when the mother was under stress. When a woman with untreated depression experienced anxiety, her heart rate rose, and her baby’s rose with her. We know that babies born to these women are highly sensitive to their environments; this could be one clue about why that is. But let me tell you–the idea of that tiny, new heart beating too fast and a fetus feeling anxiety keeps my mind open. Whatever the cost of taking medication, it’s hard to imagine that cost outweighing the benefit of keeping our fetus safe from that awful stress.